Facilitators Guide
Summary of the story
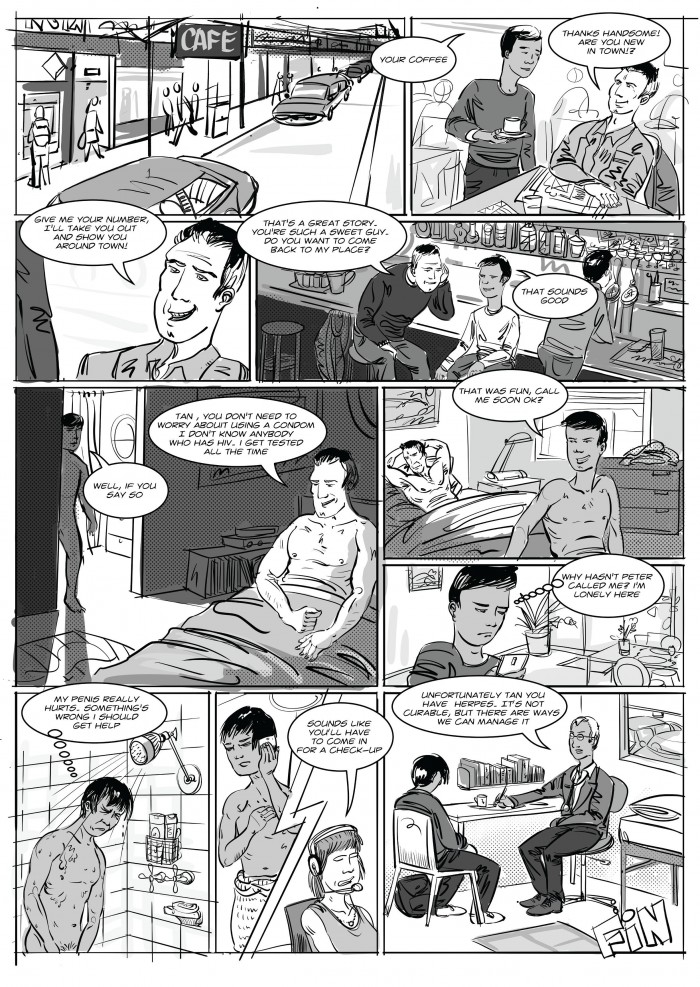
Tan is working in a café, he’s newly arrived to Australia. Tan serves Peter a coffee, and Peter offers to take Tan out. Tan and Peter go on a date and Tan goes back to Peter’s home for sex. Tan has suggested using a condom, but Peter refuses, telling him it’s not necessary. Tan is not familiar with the local sexual norms and agrees to sex without a condom because he doesn’t want to turn Peter off and is reassured by Peter that HIV is not an issue here. Tan doesn’t hear from Peter, but later starts to feel pain in his penis. He goes to see the doctor and finds out that he has herpes.
General Questions to start discussions and explore the story
- What’s happening in this story?
- Explore points that are raised by participants – ask more questions about their statements.
Hints to prompt discussion
- People who are not familiar with the sexual norms and culture of a community (in this case, the MSM (men who have sex with men) community and the local geographic community) can be vulnerable to the influence of people more experienced in that community.
- Many people try to refuse to use condoms. If given the option of sex with a condom or no sex at all, most people will agree to use a condom. It is important to be firm and insist on using a condom and water-based lubricant during sex to reduce the risk of blood borne viruses and sexually transmissible infections (BBVs and STIs).
- People sometimes lie to convince their partners to have sex with them, or do not know the facts.
- There is a power imbalance between Peter and Tan. This may affect Tan’s ability to give consent – if Tan is not familiar with the culture and norms of the community, he may not be able to give true consent.
- In Australia men who have sex with men have a higher risk of getting HIV than heterosexual sexual partners.
- You can’t tell if someone has HIV or another BBV/STI just by looking at them. Many people living with HIV or other BBV/STIs do not know they have them and may be passing them on without realising.
- Having any type of unprotected sex comes with the risk of BBVs and STIs.
- If you feel pain or notice changes in your genital area, you should go to the doctor or sexual health clinic for sexual health screening.
- If you are sexually active it is important to go for regular sexual health testing – recommendations advise men who have sex with men to go every three months for testing and other people to go every six months, even if you don’t have symptoms.
- People who are at a higher risk of HIV, can take PrEP – pre-exposure prophylaxis. This is a pill that you take once a day and can get from your doctor. It is very effective at stopping people from getting HIV when they are taking the pill every day.
- Thorne Harbour Health run workshops for gay and same-sex attracted men to socialise and learn about sexuality and well-being. The workshops are free and run by other gay and same-sex attracted men. For more information, visit their website.



 SHARE
SHARE